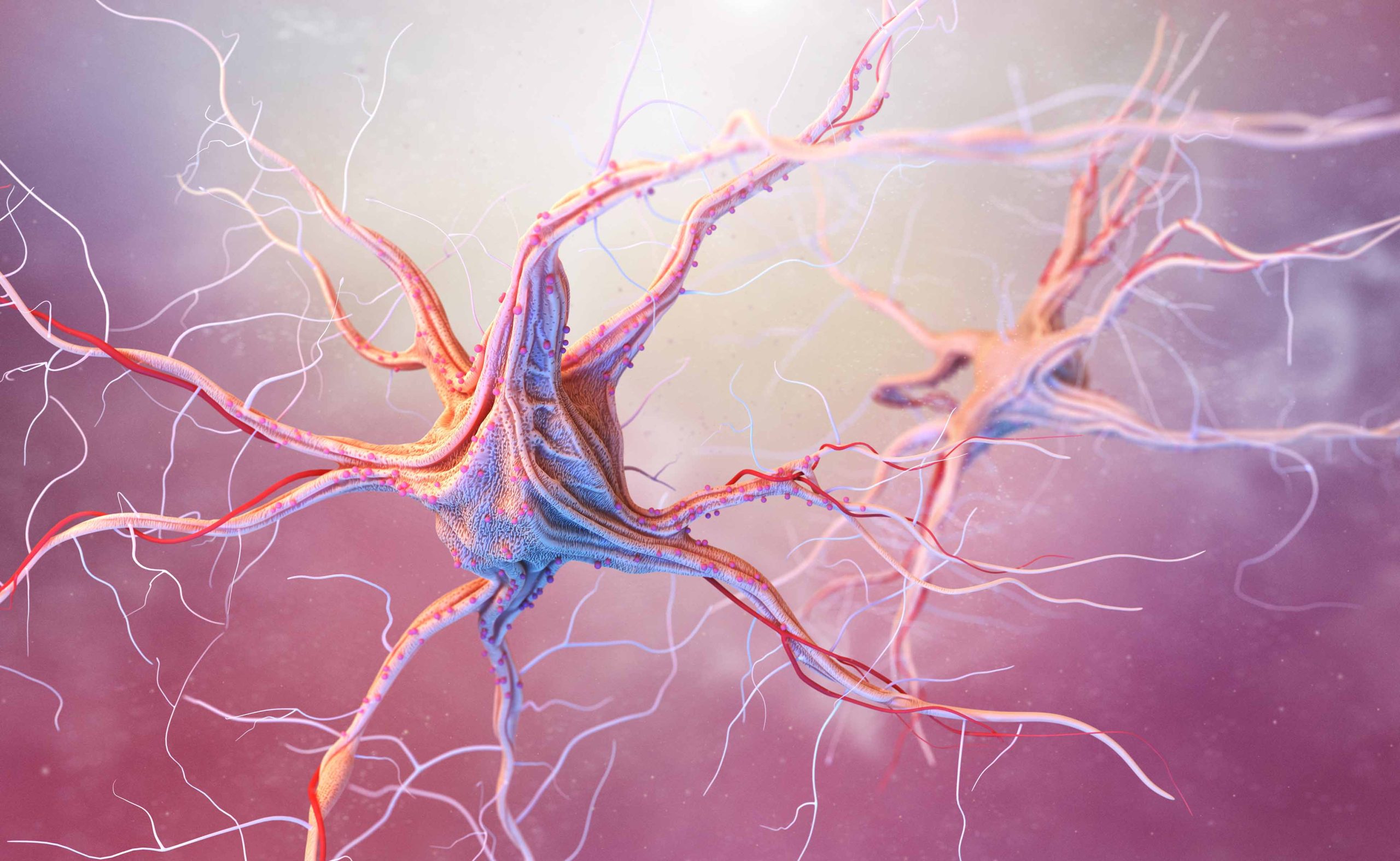
In my practice, more and more patients are asking about the relationship between digestive health and mental well-being. This growing interest is no surprise, as recent scientific findings have revealed an astonishing connection between the gut and the brain. Known as the microbiota-gut-brain axis, this interaction is reshaping how we approach mental health. Although at first glance the digestive and nervous systems seem unrelated, recent research has shown that the state of our gut microbiota can influence our mental health. This discovery opens new avenues for treating disorders like anxiety, depression, and neurodegenerative diseases. I find it particularly interesting how this knowledge could shape treatment strategies, especially as dietary and lifestyle changes are increasingly viewed as potential therapeutic tools for improving mental and brain health.
What is Microbiota and How Does It Affect Our Health?
To explore this topic, I’m first going to explain some key concepts:
- Microbiota: It refers to the population of microorganisms, like bacteria, viruses, and fungi that naturally live in various parts of the body.
- Gut microbiota: It’s the population of microorganisms that live in our intestine. Some are beneficial, others can be harmful, and others cause neither harm nor benefit. It is the most diverse and numerous microbial ecosystem in the body. It performs essential functions, such as regulating the immune system and maintaining the body’s internal balance.
- Intestinal barrier: Think of it as a protective wall lining the intestines. It controls what enters the bloodstream and what doesn’t, allowing nutrients to pass while blocking harmful bacteria and toxins.
- Blood-brain barrier: A similar protective barrier, but this one safeguards the brain, ensuring harmful substances circulating in the blood don't reach it while still allowing essential nutrients and oxygen to pass through.
- Immune system: It’s the body’s defense system. It functions like an army, identifying and attacking invaders to prevent illness.
- Hormones: These are chemical signals that travel through our bloodstream, regulating key functions in our body like growth, metabolism, mood, and how we respond to stress. They act as messengers, telling our organs and tissues when to act and how to function at the right time.
- Hypothalamic-pituitary-adrenal axis: It’s a hormonal communication system that connects the hypothalamus (a part of the brain), the pituitary gland (a gland at the base of the brain), and the adrenal glands (located just above the kidneys). This system regulates the production of cortisol, the stress hormone. When we are under stress, this axis is activated and more cortisol is produced to help us cope with the situation.
- Enteric nervous system: Often referred to as our "second brain," this network of nerves controls vital functions in our gut, like the movement of food and secretion of digestive substances. It can function independently, though it's also connected to the brain via the vagus nerve, forming a bridge between the gut and the brain.
- Neurotransmitters: These are chemical substances that act as messengers, transmitting signals from one neuron to another or from a neuron to a muscle or gland cell. They are essential for coordinating physiological and emotional functions in the body and brain.
Microbiota-gut-brain Axis
Scientific research suggests that the gut microbiota plays a significant role in regulating emotions and brain health through continuous communication between the digestive system and the brain. This ongoing interaction occurs through several pathways, including:
- Vagus nerve: This nerve carries signals both from the brain to the gut and vice versa. It allows the brain to receive information about the state of the gut and, in turn, influences its functioning, affecting digestion, intestinal movements, and nutrient absorption.
- Immune system: Our gut microbiota influences the production of cytokines, molecules that regulate inflammation. Chronic inflammation in the gut may contribute to symptoms of depression and anxiety.
- Neurotransmitters: The gut microbiota is involved in producing critical neurotransmitters like serotonin, GABA, and dopamine, which play a key role in regulating mood and mental health. What’s particularly striking is that nearly 90% of serotonin is produced in the gut, which emphasizes just how important gut health is for emotional well-being.
- Hormones: When we go through stress, the hypothalamic-pituitary-adrenal axis activates and increases cortisol production. This hormone can disrupt gut bacteria and alter digestive rhythms.
- Short-chain fatty acids: Certain gut bacteria produce short-chain fatty acids when fermenting fiber. These compounds can travel through the bloodstream, cross the blood-brain barrier, and play a role in regulating inflammation in the brain.
Dysbiosis and Factors Affecting Gut Microbiota
Dysbiosis occurs when beneficial bacteria decrease and/or harmful bacteria increase in the gut. Disruption of microbiota balance is linked to different factors: inadequate diet (high in fats and sugars, low in fiber), overuse of antibiotics, inflammatory bowel diseases, metabolic diseases, obesity, lack of sleep, substance use, intestinal infections, sedentary lifestyle, aging, certain genetic factors, and chronic stress.

Consequences of Chronic Stress on the Microbiota-gut-brain Axis
Under stress, the body releases cortisol through the hypothalamic-pituitary-adrenal axis. While this is a natural response to short-term to cope with demanding situations, prolonged stress can disrupt the balance of the gut microbiota and affect mental health. In my experience, this can lead to a cycle where poor gut health contributes to mental health issues, such as anxiety or depression, which, in turn, can worsen gut complaints.
Chronic stress can:
- Decrease the diversity of microorganisms in the gut, leading to dysbiosis.
- Alter the intestinal barrier: When the balance of the microbiota is disturbed, the intestinal barrier can become more permeable, allowing toxins and other harmful substances to enter the body.
- Cause chronic inflammation: Dysbiosis can increase inflammation and contribute to mental disorders like depression and anxiety.
- Alter neurotransmitter production: Some gut bacteria play a key role in the production of neurotransmitters like serotonin, GABA, and dopamine. An imbalance in the production of these neurotransmitters can impact mental health and nervous system well-being.
- Alter gut rhythm: Causing digestive issues such as diarrhea, chronic constipation, or other functional gastrointestinal disorders.
- Reduce the availability of nutrients to the brain.
Strategies to Improve Gut and Mental Health
1. Balanced diet:
I always recommend a diet rich in fiber, fresh foods, and fermented items, as they promote a healthy gut microbiota and, consequently, a better mental health.
- Prebiotics: These foods feed beneficial gut bacteria and are essential for maintaining balance in the gut microbiota. I suggest that patients include more fruits, vegetables, legumes, and whole grains in their diet.
- Probiotics: Probiotics are live microorganisms that, when consumed in sufficient quantities, help restore balance to the gut microbiota. They are found in fermented foods like yogurt, kefir, kombucha, and kimchi. Other sources of probiotics include apple cider vinegar, natural cider, sourdough bread, and certain aged or blue cheeses. Probiotics contribute to maintaining a healthy digestive system and strengthening the immune system.
- Healthy fats: Healthy fats, particularly those rich in omega-3, have been shown to improve the diversity of gut bacteria, reduce inflammation, and strengthen the intestinal barrier, creating a more favorable environment for beneficial bacteria. I recommend including sources of healthy fats in the diet, such as olive oil, avocados, nuts, and fatty fish, as these can support both gut health and overall well-being.
- Polyphenol-rich foods: Polyphenols, found in fruits, green tea, cocoa, and berries, serve as prebiotics and offer powerful antioxidant properties that help reduce cellular damage in the gut.
2. Physical exercise
Regular exercise is one of the most effective ways to reduce stress, improve blood circulation, and support the gut microbiota. Moderate physical activity not only helps enhance the diversity of beneficial gut bacteria but also has a direct positive impact on mood and mental health. It’s something I always recommend to my patients as part of a holistic approach to well-being.
3. Stress management
Techniques such as mindfulness, meditation, deep breathing, and yoga can help calm the mind and reduce stress levels, which in turn supports the health of the gut microbiota. Taking time each day for these practices can lead to long-term improvements in both mental and physical health.
4. Adequate rest
Proper rest and sleep are essential for mental health. Sleep allows the body to regenerate and repair, not just the digestive and nervous systems, but also the delicate balance of the gut microbiota. I often remind my patients of the importance of good sleep habits, as they play a significant role in overall well-being and support the health of both the gut and mind.

Current scientific evidence supports the idea that mental health and brain well-being are influenced by the gut microbiota through the microbiota-gut-brain axis. Factors such as a balanced diet, physical exercise, stress management, and adequate rest are essential to maintain microbiota balance and, therefore, support mental health. Since more than 25% of adults in Spain suffer from some form of mental health disorder, understanding and caring for our microbiota could be a key tool for preventing and potentially helping treating these conditions. The encouraging results we’ve seen so far in research hold promise, and I look forward to future developments that may offer new ways to improve both mental and brain health.
About the author
María Isabel Zamora is a physician with a double specialty in Psychiatry and Neurology. She has experience in the care of patients in general psychiatry consultations, and in a more specialized way, in the care of patients who combine psychiatric and neurological symptoms. She has worked with psychogeriatric patients and patients with functional diversity. She has experience in cognitive impairment, psychological and behavioral symptoms of dementia, psychiatric symptoms related to neurological disorders or chronic pain, autism, ADHD, adaptive disorders, depression, anxiety, addictions, bipolar disorder, obsessive-compulsive disorder, sleep disorders, eating disorders, etc.
Division of Medicine
Psychiatrist
Adults and adolescents
Languages: English, French and Spanish

