How Can Cognitive Behavioural Therapy (CBT) Assist Me? Unravelling the Maze of Thoughts
Imagine waking up each morning overwhelmed by a cloud of dread about the day ahead. You’re trapped in a vicious cycle of negative thoughts, each feeding into the next, building a formidable barrier between you and peace of mind. Whether it’s stress from work, anxiety about future uncertainties, or a lingering sadness that taints your enjoyment of life, finding a pathway to psychological well-being might seem akin to navigating a maze without a map.
So, what can you do? How can you break this cycle when you’re aware that your actions might be detrimental, yet you’re unsure of the alternatives? This is where Cognitive Behavioural Therapy (CBT) can make a significant difference.
What is Cognitive Behavioral Therapy?
CBT is a robust form of psychological treatment proven effective for a range of issues including depression, anxiety disorders, alcohol and drug misuse, marital problems, eating disorders, and severe psychological conditions. Extensive research demonstrates that CBT significantly enhances functioning and quality of life. It operates on the fundamental principle that our thoughts, feelings, and behaviours are interconnected, and that altering negative thought patterns can affect changes in both feelings and behaviours, and that changing behaviours can alter our feelings and negative thought patterns.
How Cognitive Behavioral Therapy Works
Many people associate therapy with lying on a couch, discussing one’s mother and traumatic past, receiving only nods or «mhms» from the therapist. However, encountering a CBT session can be quite a revelation, as it differs significantly from these traditional notions of psychotherapy. CBT sessions are interactive, practical, and structured. They focus on specific problems and offer direct tools and techniques to manage and overcome these problems. In CBT, the therapeutic process is normally divided into three key phases:
- Assessment: This initial phase involves a detailed examination of the client's problems. The therapist and client work together to identify specific problem areas. This could include understanding the situations, thoughts, and behaviours that lead to difficulties in the client’s life.
- Analysis: In this phase, there is a deep dive into understanding why these problems exist. The therapist helps the client to uncover patterns of thinking or behaving that contribute to their distress. This involves looking at how certain thoughts or behaviours are unhelpful, and exploring their origins and impacts.
- Intervention: This is the action phase, where strategies and techniques are applied to modify the problematic thoughts and behaviors. The interventions are practical exercises and tasks that the client undertakes, both within and outside of therapy sessions. These might include exposure therapy, thought records, or behavioural experiments.

For example, Ginny has sought therapy because she struggles to participate in social situations. Her job involves many important social events, and she has noticed that her inability to partake is affecting her relationships with her colleagues. She absolutely hates this and does not know how to stop being so afraid. She tried to go once. She prepaid and got ready to leave, but taking the step to leave her apartment proved too difficult, so she decided that Netflix and a glass of wine would be a better way to spend her evening, even though it felt terrible not to have been able to go.
- Assessment: The therapist and Ginny discuss everything she has been feeling, thinking, and doing when confronted with social situations to explore possible explanations for why it is too difficult to make the leap. They explore both the past and the present to understand.
- Analysis: When the CBT therapist understands what is going on, why Ginny started to struggle and why she is still struggling today, this information is shared and discussed between them. This is crucial because understanding the situation makes it easier to determine what needs to change. They do not want to guess how to intervene; they want to know.
- Intervention: Now it is time to make some changes. Ginny realizes that she anticipates a lot of negative scenarios that might occur if she goes to the party: “What if I say something weird?”, “What if my clothes are too formal or informal?”, “What if nobody talks to me, or they are bored when they do?” Her therapist helps her challenge these thoughts and prevent them from dictating her behaviour. Then, together, they create a plan to expose Ginny to what she fears the most, equipping her with all the necessary tools to manage the situation effectively.
The process of CBT is highly collaborative. Both the therapist and the client have active roles in the therapy sessions and in the work done between sessions. This collaborative effort helps to empower the client, making them an active agent in their process of change, also giving them the tools on how to manage problems in the future without the need of a therapist.
Moving Beyond the Past
While our past is crucial as it shapes who we are today, dwelling on it can impede our progress. CBT helps clients focus on the present and future, learning from the past but not being anchored by it. We discuss the past to understand our learning and experiences but shift focus to current actions and forward-looking strategies.
Benefits of Cognitive Behavioral Therapy
One of the key benefits of CBT is that it is short-term and goal-oriented, typically lasting anywhere from a few weeks to several months. We do not want to suffer longer than necessary! This does not mean the benefits are fleeting; rather, the changes are designed to be long-lasting. CBT provides clients with tools and techniques that are not just about coping in the moment but are skills that clients carry with them for life. This approach ensures that individuals do not have to rely on continuous therapy but can manage independently, reducing the likelihood of future relapses. The benefits of CBT include:
- Evidence-Based: CBT's effectiveness is backed by substantial research, making it a reliable form of therapy for various psychological problems.
- Skill Development: Clients acquire valuable life skills that enable them to effectively tackle a variety of life's challenges. These skills, learned within the therapy setting, can be generalised to address similar issues that may arise in the future.
- Sustainability: While the therapy itself is often short-term, the tools and strategies learned are enduring, helping ensure that the improvements are maintained long term.

Embracing Negative Emotions
Even though CBT talks a lot about change, it is essential to acknowledge that feeling bad is sometimes necessary. Negative emotions are a normal part of life; they teach us resilience and give context to our happiness. How would we recognise joy if we never experienced hardship? How would we handle danger without fear? Thus, not every problem requires therapy – many challenges can be managed on our own, even though we feel bad in the moment. However, when these issues persist and begin to impact our daily lives significantly, seeking therapy may be the appropriate step to take, and this is when CBT would be able to help us.
Sinews MTI
Psychology, Psychiatry and Speech Therapy
Evolution of Transsexuality-Related Diagnoses
DISCLAIMER: This article contains obsolete language that stems from the pathologization of realities that in no case are considered disorders by any reputable Psychology or Psychiatry institution, both at a national and international level. The language used in this article reflects the evolution of academic and health institutions throughout history and it is included here to reflect how the approach of institutions to social demands influences the categorization of the realities studied.
This article is a continuation of the one I recently published on the historical evolution of the diagnoses that the American Psychiatric Association attributed over the years to people with a non-normative sexual orientation. That is, with a sexual orientation other than heterosexuality.
The previous article would not make much sense if I did not also publish this one right after it, as the goal behind writing both of them is to observe how the evolution of the different diagnoses that have been assigned to people with non-normative sexual orientations is surprisingly similar to that of diagnoses assigned to trans people.
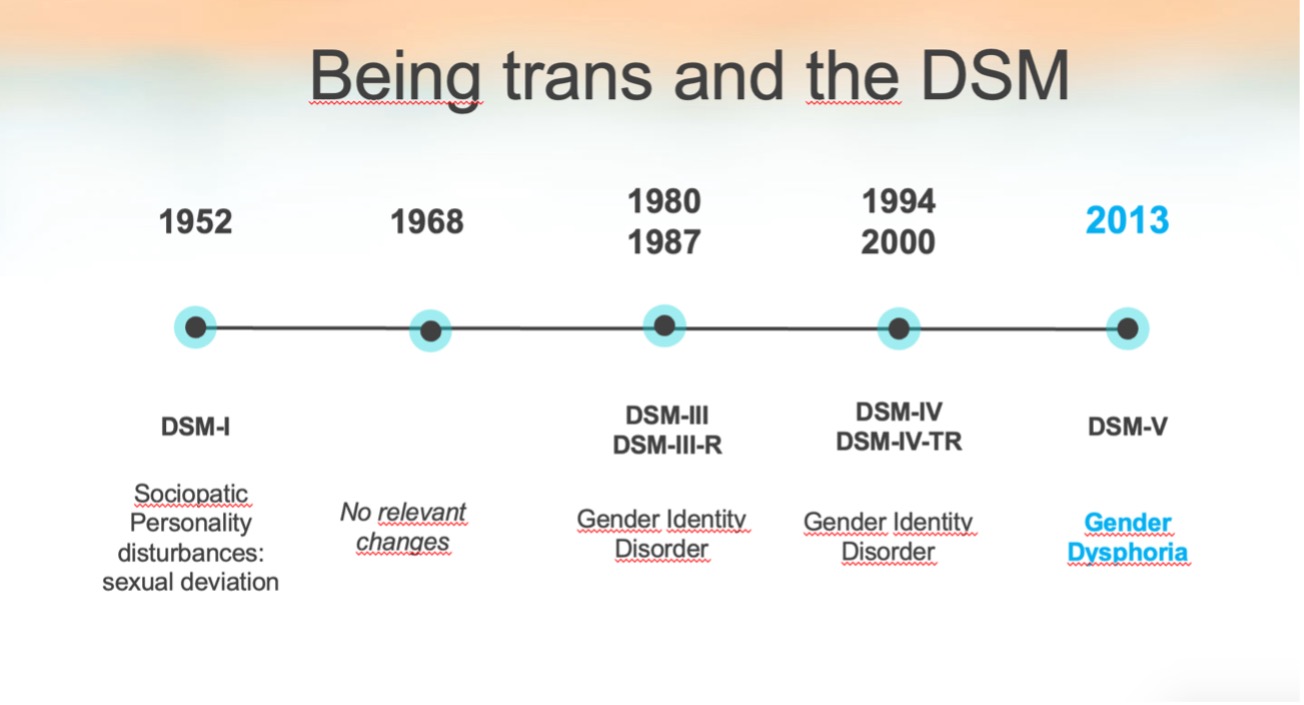
Evolution of Transsexuality-Related Diagnoses in the DSM Manuals of the American Psychiatric Association
As in the previous article, I will now review the different diagnoses that the American Psychiatric Association has assigned to trans persons throughout the different editions of the DSM.
DSM-I (1952)
The first edition of the DSM does not explicitly mention transsexuality.
DSM-II (1968)
DSM-II proposes a category for Sexual Disorders, although it is limited and mostly focused on homosexuality and other “disorders of sexual deviance”. Transsexuality is not separated from other realities, but different forms of gender role nonconformity were broadly encompassed as Sexual Deviance.
DSM-III (1980)
DSM-III represented a significant change by introducing for the first time the term “Gender Identity Disorder” (GID), defined as a persistent incongruence between biological sex and the person’s experienced or expressed gender identity. This was an early attempt to formally recognize transsexuality within a clinical framework.
The diagnosis of GID was classified under a new chapter called “Psychosexual Disorders,” which also included other disorders related to sexuality. However, this classification was criticized for pathologizing gender identity not congruent with the sex assigned at birth.
DSM-III-R (1987)
In the revised version of DSM-III (DSM-III-R), the diagnosis of Gender Identity Disorder was maintained, but some modifications were made to the diagnostic criteria. Transsexuality was still seen as a mental disorder.
DSM-IV (1994)
In DSM-IV, Gender Identity Disorder is retained, but distinctions are added for evaluations in children, adolescents and adults. This category caused controversy because of the implication that gender variants in childhood were seen as pathological.
DSM-IV-TR (2000)
The DSM-IV was revised in 2000. The diagnosis of “Gender Identity Disorder” was maintained with some modifications, maintaining the categories and criteria established in the previous version. The manual was still under criticism from the trans community and activists for continuing to include trans realities within pathologizing labels.
DSM-5 (2013)
The publication of DSM-5 marked a major shift in how the American Psychiatric Association addresses transgenderism. The term “Gender Identity Disorder” was replaced with “Gender Dysphoria.” This change is exposed as an effort to reduce the stigma associated with the diagnosis by emphasizing that it is not the gender identity itself that is problematic, but the significant distress that a trans person may experience in the current context.
In addition, the DSM-5 introduced more detailed diagnostic criteria, differentiating gender dysphoria in children from that experienced in adolescents and adults. It was also explicitly recognized that not all people with gender incongruence experience significant dysphoria, in order to clarify that transsexuality is no longer inherently viewed as a mental disorder.
DSM-V-TR (2022)
The DSM-5-TR (Diagnostic and Statistical Manual of Mental Disorders, Revised Text) represents a revision of the DSM-V, adding minor changes to the 2013 edition, including some key changes regarding gender dysphoria to reflect greater accuracy and awareness of the social reality being discussed:
- The term “desired gender” has been replaced with “experienced gender,” underscoring that gender identity is an internal experience and not just a desire for change.
- The phrase “medical cross-sex procedure” has been updated to “gender affirming medical procedure,” reflecting a more respectful and affirming approach toward medical interventions related to gender identity.
- Language regarding sex assigned at birth has been modified. The terms “natal male” and “natal female” are now described as “person assigned male at birth” or “person assigned female at birth,” reinforcing the distinction between assigned sex and experienced gender.
Future Perspectives
The evolution of transgender-related diagnoses in the DSM manuals reflects an ongoing process of revision and updating as understanding of gender diversity advances. It is expected that future revisions will continue to depathologize trans identities and focus more on providing a supportive framework for those experiencing gender dysphoria, rather than classifying them within a pathological context.
The current category of “Gender Dysphoria” is not without controversy as it receives similar criticism as the category of “Egodystonic Homosexuality” did at the time. There are also arguments, of a more practical nature, in favor of it because of the requirement of insurers and health services for the presence of a diagnosis that justifies gender reassertion interventions in trans persons. However, some argue that there are already natural conditions, such as pregnancy, that require medical interventions without the need for a pathologizing diagnosis, so the same logic could be applied to interventions aimed at improving the quality of life of trans people.
About the author
Jorge Jiménez Castillo is a psychologist at SINEWS, where he practices in English and Spanish. He works daily with local and international populations and has a long history of studying the reality of the LGTBIQ+ community in and out of the clinic. He works from a cognitive-behavioral approach with evidence-based interventions and believes that in order to provide quality psychological care one must be aware of the inequalities that intersect with users and explore how they intersect with each other.
Sinews MTI
Psychology, Psychiatry and Speech Therapy
The journey to clear communication: Improve your accent
Communication is the expression of a message by speaking, writing, or signing. When a message is not expressed clearly, it can be misinterpreted. Clear communication means that the receiver of the message understands exactly what the sender is intending. It is essential for being understood, building relationships, and communicating efficiently.
For many Spanish speakers, having clear communication when speaking English can be an important step when it comes to achieving their goals, whether that be in their careers, their social lives or just not having to repeat themselves and being understood. The purpose of accent training is to help you feel confident and to communicate as effectively as possible—not to sound like a native speaker or erase your individuality. This in-depth guide will go over what accent training is, how it works, and how one-on-one coaching can help with clarity, confidence-building, and successful communication in both professional and social settings.
What is Accent training?
Accent training is personalized coaching that helps individuals who want to address specific communication challenges. It focuses on pronunciations, appropriate intonation, rhythm, timing, and stress patterns. It helps speakers identify which habitual features they take from Spanish and use while speaking English. The goal of accent training is not to sound like a native speaker, it is to help individuals communicate clearly and confidently. Accent training is flexible and personalized to meet each individual’s needs.

What are accents?
Accents are made up of substitutions; the sounds, rhythms, and intonations from a person’s native language or region that he or she uses when speaking English. If these substitutions are not what the listener expects to hear in English, the listener hears an accent (The accent channel). Accents are a normal part of any language and reflect the cultural diversity of speakers. No accent is better than another; they are all valid forms of expression.
Accents only become noteworthy if they begin to interfere with someone’s communication at work or in social settings. They may cause confusion or prevent someone from achieving their goals. Some people may also feel that there are preconceived notions about their accent, which can lead to biases and stereotypes. The choice to change the way we speak is up to each individual. They may want to improve their communication and avoid embarrassing speech mistakes.
After accent training, most accents become difficult to associate with any specific location; they begin to sound very neutral and unidentifiable. Speakers become easily understood, which boosts their confidence and allows them to communicate clearly and as effectively as possible.
Benefits of Accent Training:
- Aids in clearer communication and pronunciation.
- Helps individuals work towards their career, social network, and life goals.
- Increases confidence and self-esteem.
- Reduces linguistic bias and discrimination.
- Improves customer satisfaction.
- Enhances listening skills.
- Expands professional opportunities.
- Nurtures better social integration.
- Increases cultural sensitivity and the ability to connect with diverse backgrounds.
- Improves credibility in professional settings.
- Decreases stress levels associated with speaking in a foreign accent.
- Enhances academic performance for students by facilitating participation in discussions and presentations.
- Strengthens personal relationships by reducing misunderstandings and fostering clearer interactions.
- Empowers individuals by giving them a sense of control over their communication and self-presentation.

Why personalized training instead of apps and videos?
Personalized accent training provides many advantages over apps and videos. It offers immediate feedback and allows the opportunity to correct mistakes instantly. It also helps the individual to recognize their personal challenges when communicating; not every Spanish speaker has to work on the same objectives during accent training. Unlike apps and videos, personalized training is tailored to each individual’s needs. Working with a speech trainer also ensures you are accountable and practicing consistently, which is important for progress. Immediate feedback from a speech trainer is much more effective and leads to better results.
The accent training process
The process of accent training begins with a speech assessment in order to identify the sound substitutions, rhythms, stress patterns, and intonations that are currently being used and would need to be replaced with those of the goal accent (General American English for example). Once the substitutions are identified, appropriate objectives can be set. It is important to note that new objectives may appear after the initial assessment as the speech trainer is constantly assessing their client as they work together. Each session targets a single objective and consists of a variety of tasks that are practiced multiple times. During these tasks, immediate feedback is given to help the client identify any substitutions and make the necessary corrections. In addition to these in-session practices, at-home tasks are assigned; it is crucial that the client practices consistently outside of sessions in order to make notable progress. Repetition is necessary for making adjustments in the accent, and frequent practice is required for permanent improvement. The goal of accent training is for the client to internalize the correct speech patterns and produce them fluently in a way that is easily understood by their listeners.
How long will it take?
Each goal takes approximately one session to be taught. It is recommended to have one session a week, and normally takes between 12-15 sessions to work through each objective (depending on the number of objectives of each student, could be more, could be less). It is important that the student is practicing at home at least 15 minutes a day to make notable progress. After the completion of their program, the client will have the option of maintenance sessions if they would like to continue practicing with a speech coach.

What will we work on?
To communicate clearly and confidently, we will focus on several key areas tailored to each client’s needs. We will address high-value sounds specific to English that are uncommon in Spanish and can lead to pronunciation difficulties. We will also work on rhythm and stress; English features vary in syllable length, some syllables are stressed and longer, while Spanish syllables are generally given equal time. Additionally, we will focus on vocabulary, predominantly common words used in daily life that are often mispronounced. We will use targeted exercises and practice to improve pronunciation, rhythm, and vocabulary, which will enhance overall communication skills.
Taking action to overcome communication challenges is an important step towards personal and professional development. Accent training is a powerful tool that can help you achieve effective and clear communication. It can help boost your confidence and enhance your interactions in all areas of life. Working with a speech trainer provides you with personalized guidance and support, and ensures that you reach your goals more effectively than through self-study tools alone.
About the author
I am Jarrisvette Villarreal, originally from South Texas. I have been living in Spain for several years, where I have worked as an English teacher and have taught young Spanish speakers. Through my experience, I have become familiar with the common mispronunciations and typical mistakes Spanish speakers make when speaking English. In addition to teaching, I have experience as a Speech-Language Pathologist Assistant, working with children on articulation through speech therapy. I have also completed a specialized training in accent coaching through “The accent channel”, which has equipped me with the skills to provide personalized accent training. I have also worked diligently to achieve a neutral English accent; I understand the challenges and preconceived notions about having an accent. I am passionate about teaching pronunciation and excited to help others reach their communication goal.
Sinews MTI
Psychology, Psychiatry and Speech Therapy
How to Prepare Our Children for Life's Ups and Downs
What wouldn’t we do to protect our children, our most precious treasures? As parents, our instinct is to shield them from harm and negative experiences, fearing that difficult situations might cause pain or lasting trauma. We are driven by love and a deep desire to see our children happy and thriving. However, in our efforts to safeguard them, we might unintentionally prevent them from developing the resilience they need to navigate life’s inevitable challenges.
The Importance of Facing Challenges
Resilience is the ability to bounce back from adversity and cope with setbacks. It is a crucial skill that helps children manage the complexities of life. Shielding them from every challenge can leave them unprepared for future difficulties. Without encountering adversity, they may struggle to handle setbacks when they arise, potentially leading to a lack of confidence and problem-solving abilities.
Understanding and Accepting Emotions
One of the most valuable lessons we can teach children is that emotions—both positive and negative—are a natural part of life. Everyone experiences anger, frustration, or sadness at times, and that’s okay. Emotions are natural responses to situations and are not something we can directly control, but we can control how we express and respond to them.
It’s essential for children to understand that feeling sad, frustrated, or angry is perfectly normal. These emotions aren’t to be feared or avoided; rather, they are signals that deserve attention. For example, fear can alert us to danger, such as encountering a wild animal (we do not want to meditate when a lion is approaching us), prompting us to take protective action. Anger, when managed properly, can help us stand up for ourselves and advocate for a just world (we do not want to be taken advantage of). By teaching children to accept their emotions, rather than suppress or ignore them, we help them develop an understanding of their emotional responses—a cornerstone of resilience.
Teaching Healthy Emotional Expression
While understanding emotions is crucial, it’s equally important for children to learn how to express them in healthy and constructive ways. We cannot always run away from what scares us, nor can we lash out when angry. It is okay to feel emotions, but how we express them matters. Children need to learn effective ways to manage their emotions so they do not create new problems, which could intensify their negative feelings.

How Can I, as a Parent, Teach My Child to Cope with Negative Emotions Without Causing Trauma?
First, remember that your child is a keen observer. One of the most powerful ways they learn is by watching your behavior. If you model healthy emotional expression, your child is likely to emulate it. Conversely, if you respond to anger by hitting or breaking things, it becomes difficult for the child to understand that these behaviors are unacceptable.
A helpful guideline is to focus on teaching your child what to do, rather than what not to do. Instead of saying “Don’t hit” or “Don’t scream,” guide them toward alternative behaviors. For example, you might say, “I see you’re angry because of what happened. It’s understandable—it’s not fun when things don’t go your way. When you’re angry, use your words to tell me what’s bothering you, and we can figure out how to make things better.” This approach is easier said than done, especially when parents are short on time and energy. Many of us weren’t taught how to manage our own emotions, so learning to do so may be necessary before we can effectively teach our children. Remember, just like on an airplane, you need to put on your own oxygen mask before helping others.
Here are some strategies to help children manage and express their emotions effectively:
- Model Healthy Emotional Expression: Children learn by observing the adults around them. Demonstrate healthy ways to express emotions, such as calmly discussing what’s bothering you instead of yelling. This shows children that emotions can be managed without resorting to negative behaviors.
- Encourage Open Communication: Create an environment where your child feels safe to talk about their feelings. Encourage them to express what they’re feeling and why without fear of judgment. Listening actively and empathetically to their concerns helps them process emotions and strengthens their ability to communicate effectively.
- Teach Problem-Solving Skills: When children face challenges, guide them in thinking through possible solutions rather than stepping in to fix the problem for them. Encourage them to consider different approaches and evaluate potential outcomes. This builds their confidence and empowers them to tackle challenges independently.
- Set Healthy Boundaries: While all emotions are valid, there are appropriate ways to express them. Set clear boundaries around acceptable behaviors and help children find constructive outlets for their emotions, such as talking or engaging in physical activities.

Preparing Children for a Resilient Future
Building resilience in children doesn’t mean exposing them to unnecessary hardships; rather, it means equipping them with the tools they need to handle the challenges they will inevitably face. By teaching them to understand, manage, and express their emotions, we prepare them for the realities of life and help them build the resilience needed to thrive.
Resilient children are better equipped to cope with adversity, recover from setbacks, and continue moving forward. They understand that emotions are a natural part of life and that challenges, while difficult, can be managed. With these skills, they will be prepared to handle criticism at work or navigate conflicts in their personal relationships, confidently facing whatever life throws their way.
Sinews MTI
Psychology, Psychiatry and Speech Therapy
The Importance of Connection, Rhythm, and Intonation in Accent Training
Accent training is a specialized form of language instruction designed to help individuals modify or refine their accent in a second language. It goes beyond working on your pronunciation and perfecting the sounds of individual words; it also involves the way we connect words, the rhythm, and the intonation that we use when speaking. Many speakers unknowingly carry over the speech patterns of their native langue when speaking English, this can sometimes change the meaning of what is being said and affect clarity. Personalized Accent training can pinpoint the specific aspects of speech a person may need to target, to ensure that they are conveying a clear message. This guide will explore how connection, rhythm, and intonation are essential to accent training and how they can help anyone who wants to sound more natural and confident when speaking English.
Who can benefit from accent training?
- Non-native speakers who want to improve their clarity and confidence when speaking a second language, particularly in professional, academic, or social settings.
- Professionals who need to communicate clearly with native speakers for work, such as in international business or customer-facing roles.
- Actors or performers who need to adopt a specific accent for a role.
- Anyone who feels their accent may be a barrier to effective communication or integration into a new language environment.

Why Focus on Connection, Rhythm, and Intonation?
Mastering connection, rhythm, and intonation is crucial for achieving natural and fluent English speech. While pronunciation is foundational, these elements ensure that speech flows smoothly and conveys intended meanings accurately. Effective accent training emphasizes these aspects to help non-native speakers overcome the influence of their native language and sound more natural in English.
Connection in Speech
Connection in speech refers to the way we blend words and sounds to create fluent communication. Without these connections, speech can sound unnatural or choppy, making non-native speakers come across as robotic. English speakers often link words that start with consonant sounds or blend vowel sounds between words, such as in phrases like «turn off» (which can sound like «turnoff») or «see it» (which can sound like «seeyit»). Enhancing how you connect sounds can improve pronunciation, rhythm, timing, and overall intelligibility. When speaking English, it is important to connect words smoothly so that entire sentences flow together. Pausing is natural and appropriate at the end of a sentence, when taking a breath, or when emphasizing a particular point.
Rhythm in Speech
Rhythm in speech plays an important role in effective communication. It involves the patterns of stressed and unstressed syllables and influences how messages are perceived. People are accustomed to hearing a certain timing during speech to fully comprehend a message. When the rhythm is off, the message can be difficult to follow or can cause confusion. “English is a stress-timed language, meaning, we don’t give equal stress to every syllable, but we spend lots of time on some syllables and we rush through other syllables” (The accent Channel). In English, when stressing a syllable, the vowel becomes longer, louder, and goes up in pitch. This can make it challenging for Spanish speakers to adapt to uneven stress patterns and can affect the natural sound of their speech.

Intonation in Speech
Intonation in speech refers to the variation in pitch that we use to convey different meanings in English. It helps distinguish between statements, questions, and commands. Intonation can also reveal emotions like sarcasm, uncertainty, or enthusiasm, and it highlights important aspects of a spoken message. When we vary in pitch, we can express a range of meanings and emotions.
Spanish speakers sometimes use repetitive intonation patterns when speaking English, this can make a person sound monotone and confusing. Without proper intonation, speech is flat and difficult to follow. Stressing different parts of a phrase can completely change its meaning, even when using the same words. Mastering intonation is crucial for clear and engaging communication.
Differences Between English and Spanish in Connection, Rhythm, and Intonation
English and Spanish differ significantly in their approach to connection, rhythm, and intonation. Spanish, being a syllable-timed language, maintains a steady rhythm by giving equal time to each syllable. In contrast, English’s stress-timed nature creates a more fluid and varied rhythm, with stressed syllables occurring at regular intervals. This difference can lead Spanish speakers to emphasize every syllable equally in English, disrupting the natural rhythm and clarity of their speech.
When it comes to connection, Spanish tends to maintain a more continuous flow between syllables, with each sound clearly articulated. English, however, often blends sounds together, making it sound smoother and more connected. Additionally, while Spanish vowels are precise and static, English vowels are longer and more dynamic, requiring greater mouth movement. Finally, when Spanish speakers speak English, they tend to use a repetitive intonation, and English requires varied intonation to convey different emotions and intentions. By focusing on these differences—strong syllables, elongated vowels, varied intonation, and fluid sound connections—Spanish speakers can significantly improve their clarity and fluency in English.

How a Speech Coach Can Help
A speech coach is essential for mastering connection, rhythm, and intonation which are critical for natural English communication. Through tailored exercises and real-time feedback, a coach can address specific challenges in blending words, managing syllable timing, and varying pitch. Coaches use practical techniques, such as listening drills and rhythmic practice, to improve speech flow and intonation. Personalized training ensures that learners understand and apply these elements effectively, leading to more natural and confident speech.
Mastering connection, rhythm, and intonation is essential for anyone looking to improve their English accent and communicate more effectively. These elements are the building blocks of natural speech, influencing how we are understood and how our messages are received. While pronunciation is important, it is the fluidity of connected words, the rhythmic flow of stressed and unstressed syllables, and the dynamic use of pitch that makeup language.
For non-native speakers, especially those coming from languages with different speech patterns like Spanish, focusing on these areas can make a significant difference in how natural and confident their English sounds. With the help of personalized accent training and a speech coach, learners can develop these skills, leading to clearer, more engaging communication. Whether for personal growth, professional development, or social interaction, refining connection, rhythm, and intonation can unlock a new level of proficiency in English, helping speakers to be not only understood but also to connect more deeply with others through language.
About the author
I am Jarrisvette Villarreal, originally from South Texas. I have been living in Spain for several years, where I have worked as an English teacher and have taught young Spanish speakers. Through my experience, I have become familiar with the common mispronunciations and typical mistakes Spanish speakers make when speaking English. In addition to teaching, I have experience as a Speech-Language Pathologist Assistant, working with children on articulation through speech therapy. I have also completed a specialized training in accent coaching through “The accent channel”, which has equipped me with the skills to provide personalized accent training. I have also worked diligently to achieve a neutral English accent; I understand the challenges and preconceived notions about having an accent. I am passionate about teaching pronunciation and excited to help others reach their communication goal.
Sinews MTI
Psychology, Psychiatry and Speech Therapy
What is Speech and language therapy?
Speech therapy is the branch of science that focuses on the assessment, diagnosis, treatment and prevention of speech, language, communication and swallowing disorders. It is a discipline that serves people of all ages. Speech therapy is a profession that combines different areas, such as linguistics, psychology, biology and medicine.
In America, the Spanish Association of Speech Therapy, Phoniatrics and Audiology (AELFA-IF) is one of the main organisations of speech therapists in Spain. This association offers resources, ongoing training and support to professionals.
Areas of intervention in speech therapy
Speech therapists can work in a wide variety of settings, such as hospitals, private clinics, schools, nursing homes and early childhood centres, among others. Areas of intervention include:
- Speech disorders: this group of disorders encompasses difficulties in producing speech sounds, such as stuttering, dysarthria and articulatory disorders.
- Language disorders: this group of disorders encompasses difficulties in the comprehension and production of language, both written and oral. Within language disorders, we can distinguish expressive disorders, i.e. those that consist of difficulties in expressing oneself, and receptive disorders, which are characterised by difficulties in understanding the message.
- Social communication disorders: these are disorders that involve difficulties at the pragmatic level, i.e. with the use of language. They usually occur in social communication and are characterised by difficulties in communication skills. Communication skills are understood as those skills that are put into action and allow for an effective exchange between two or more people.
- Within these skills we can distinguish: the ability to communicate assertively, the ability to communicate a specific message, the understanding of non-verbal language, the ability to develop active listening, etc.
People with social communication disorders show difficulties in using these skills effectively. - Voice disorders: these are pathologies that involve vocal difficulties. This group includes problems such as aphonia (absence of voice) or dysphonia. These disorders are characterised by an impairment of the quality, tone and volume of the voice.
- Swallowing disorders: these disorders are commonly known as dysphagia and affect a person's ability to swallow. They may be caused by neurological disease, injury or surgery.

Speech therapy as evaluation
As mentioned above, speech therapy also encompasses the area of assessment. This is a multi-stage process. Speech therapists use techniques and tools to assess speech, language, communication and swallowing. Assessment can be carried out through standardised or non-standardised tests.
The first step in an assessment is an initial interview, in which detailed information about the patient’s development is collected. It is important to know the patient’s medical history and family history. In addition, it is very important to know about possible speech and language difficulties.
After this first step, assessment takes place. This may be through standardised tests, with specific tests that compare the individual’s performance in a given area with the norms established for their age group, or through non-standardised tests, which include observation of the user in their daily life or in specific activities to assess specific aspects.
This assessment allows the identification of the strengths and weaknesses of individuals, which enables the setting of specific goals for therapeutic intervention.
With the information extracted from the assessment, the speech therapist establishes intervention objectives. These goals can be short, medium or long term and allow the user’s progress to be monitored.
- Articulation disorders: the exercises that are implemented in therapy to treat these difficulties are focused on learning the way and place of articulation of sounds, to improve the emission of sounds, as well as exercises to improve the clarity of speech.
- Language disorders: Exercises to target language disorders are aimed at improving language comprehension and production. They may also focus on improving pragmatic and social skills.
- Voice disorders: to treat vocal difficulties, users learn techniques to improve breathing and phonation. These exercises improve their vocal quality.
- Swallowing disorders: THE intervention in this group of disorders is aimed at the user learning strategies to improve swallowing safety and efficiency. Exercises to work on the tone of the facial muscles, changes in diet and learning safe swallowing techniques can be found.

Recent advances in speech therapy
Speech therapy intervention is a dynamic process, i.e. it is subject to change, as each person has specific needs. It will be up to the professional who takes the individual to make these adjustments to the initial plan. This will be done on the basis of how he/she sees the individual in the sessions.
Speech therapy is a fairly new science. Moreover, it is a field that is continually evolving, which is why research within speech therapy is so important. Some of the recent advances are:
- Neuroplasticity: this is research into how the brain can reorganise its connections and form new connections in response to therapy.
- Genetics: research within genetics allows for the exploration of the transmission of different disorders and the observation of whether genetic inheritance influences the transmission of these disorders to offspring, as well as the likelihood of their occurrence.
- Evidence-based intervention: research allows for the development of new therapeutic practices. This allows speech therapists to implement these new techniques in their intervention, with the advantage of ensuring that they are effective and efficient treatments.

As a general conclusion, speech therapy is a profession that treats disorders related to speech, language, communication and swallowing through individualised intervention. The goals of the intervention are established on the basis of an exhaustive assessment carried out by the professional. The speech therapist has a very important role in improving the quality of life of individuals in need and seeks to develop skills and tools that enable people to communicate effectively.
It is an area in which research plays an important role in incorporating new techniques into interventions, ensuring their effectiveness.
Some sites that provide up-to-date information on speech therapy are:
- American Speech-Language-Hearing Association
- National Institute on Deafness and Other Communication Disorders
- Speech-Language-Therapy.com
- Understood
Written by:
Mariló Martínez
Sinews MTI
Psychology, Psychiatry and Speech Therapy
Evolution of Homosexuality Diagnoses
DISCLAIMER: This article contains obsolete language that stems from the pathologization of realities that in no case are considered disorders by any reputable Psychology or Psychiatry institution, both at a national and international level. The language used in this article reflects the evolution of academic and health institutions throughout history and it is included here to reflect how the approach of institutions to social demands influences the categorization of the realities studied.
As is often the case with ideas that seem to be my own, it is not clear to me whether the thoughts underlying this article – and the next one that I will publish as a continuation of it – are homegrown or the result of having read about them somewhere. Probably the latter, hence why I am very grateful to all those who write about human rights and the importance of ethical practices within institutions. It has long been clear to me that being original is wildly overrated. If someone has good ideas, it is better to listen to them, internalize them and elaborate on them so that you can expand them in a way that makes sense within your own worldview and, in my case, the scientific evidence available to me. I apologize for not citing authors in these articles, but it is difficult for me to point to anyone specific. However, I would like to briefly mention Devon Price, a social psychologist who does an incredible job at educating and advocating for human rights. It may seem unexpected that I, as a Psychologist doing therapy at a clinic, would mention a Social Psychologist as an author I resort to for relevant topics about my work. However, because of my eagerness to do evidence-based work, Behavior Analysis is central in my practice because this approach, even if heavily misunderstood, is focused on the interaction between a person and their environment. Therefore, Social Psychology is perfect if I want to broaden my understanding of how our context shapes our reality.
Since it dawned on me, I periodically catch myself thinking about how the evolution of the diagnostic labels attributed to the realities of trans people is strikingly similar to that of the labels attributed to people with non-normative sexual orientations. The depathologization of non-heterosexual people is widely accepted by all institutions of psychology and medicine, but although the depathologization of trans people follows the same path, we have not yet reached the completion of that process in part due to, I believe, the fact that society has not yet finished understanding and accepting the existence of people who identify with a gender other than the one assigned at birth based on their genitalia.
The diagnoses included in the DSM (Diagnostic and Statistical Manual of Mental Disorders, published by the American Psychiatric Association) and other classifications are a product of their time, as they reflect the interests of society and the paradigms most accepted by psychiatrists at the time of their publication. Thus, I have decided to show the evolution of both diagnoses assigned to homosexuality (and other non-heterosexual sexual orientations) and those assigned to trans people.
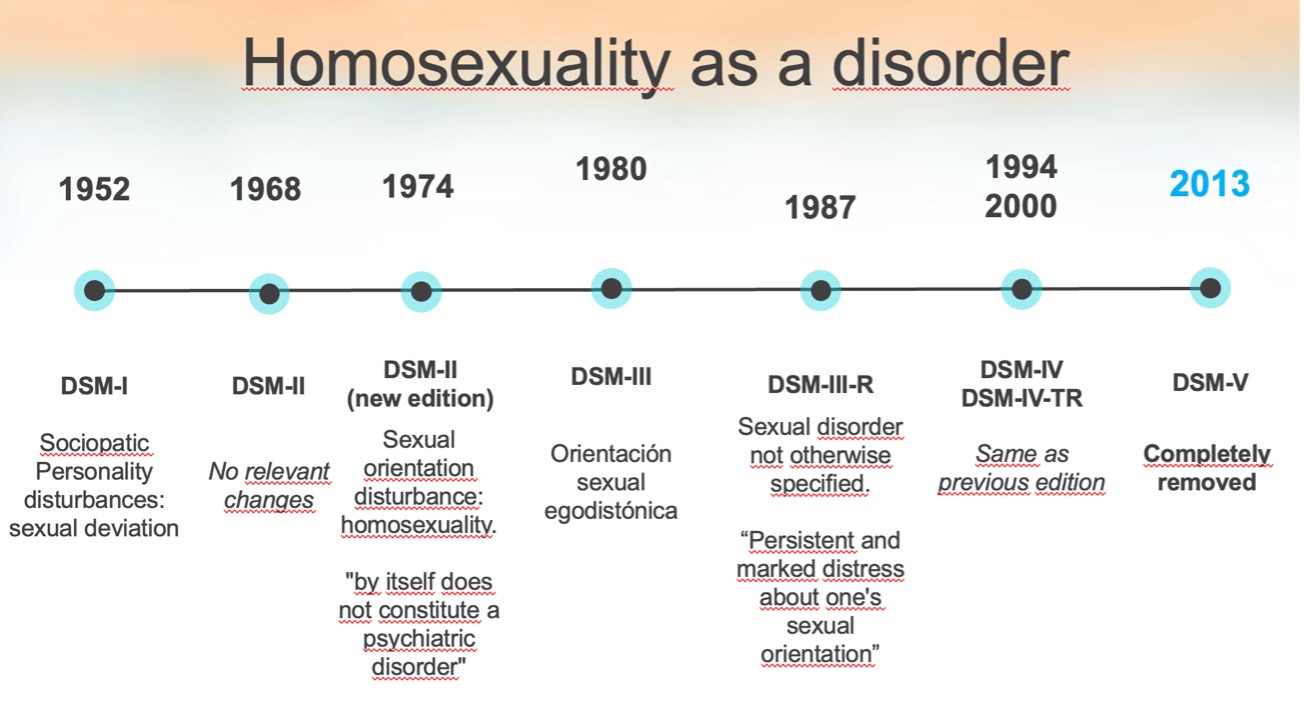
Evolution of Diagnoses Associated with Homosexuality
Different editions of the Diagnostic and Statistical Manual of Mental Disorders (DSM) have classified homosexuality differently, reflecting changes in the social perception of homosexuality over time.
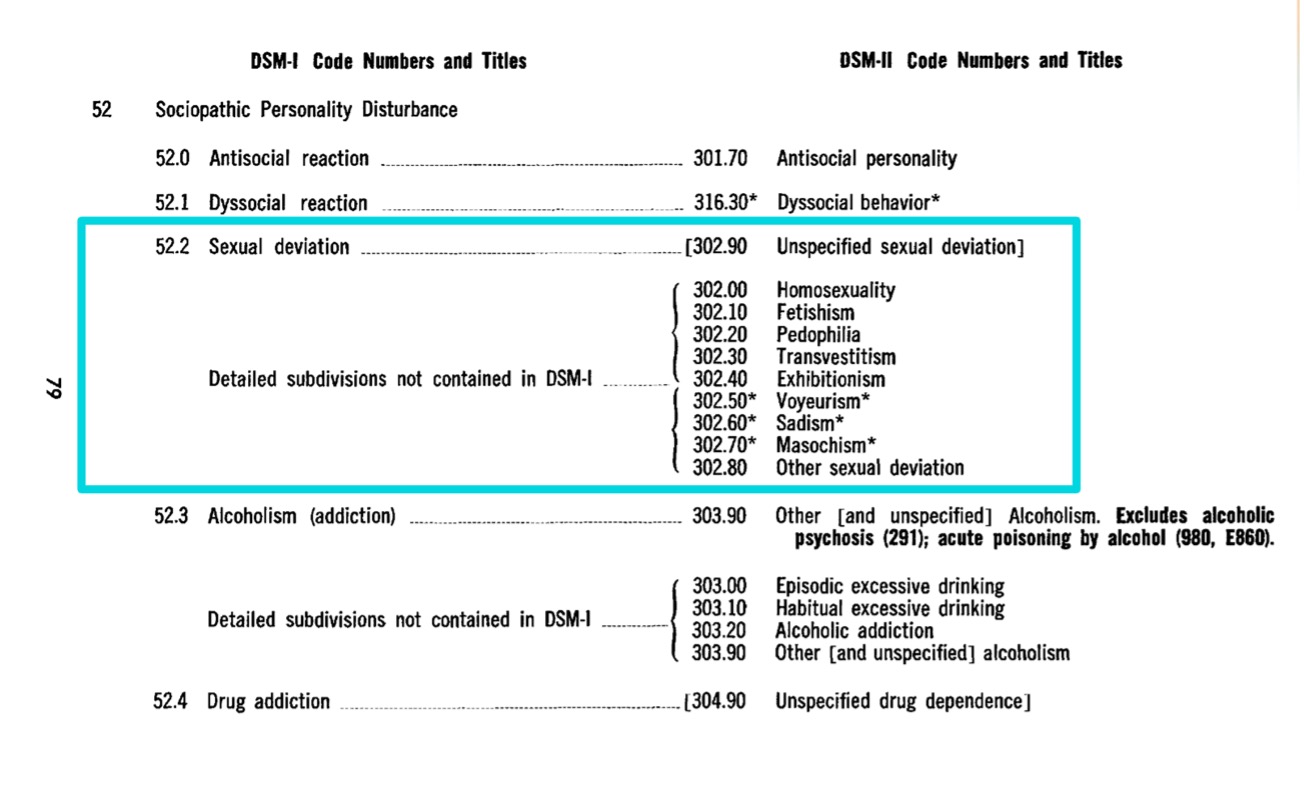
DSM-I (1952)
“Sociopathic Personality Disorder – Sexual Deviations”: In the first edition of the DSM, written in 1952, homosexual people are diagnosed with a “Sociopathic Personality Disorder”, within the subcategory of “Sexual Deviations”, reflecting a clear negative bias towards this population.
DSM-II (1968)
Homosexuality is still included under “Sexual Deviations”. However, this time there are a bunch of other subcategories classified as sexual deviations along with it. Thus, homosexuality appears in this edition along with other categories such as fetishism, tavestism, pedophilia and sadism, among others.
Strong criticism from society: During the 1960s and early 1970s, and due to a growing civil rights movement and pressure from LGBT activists, ordinary people and professionals begin to talk about the need for the elimination of homosexuality as a psychiatric diagnosis.
Removal of Homosexuality from DSM-II (1973):
In 1973, the Board of Directors of the American Psychiatric Association (APA) makes the decision to remove homosexuality as a mental disorder after voting on it. In its place a new category is created: “Disorders of Sexual Orientation,”. This new label does not present homosexuality as a disorder in itself, but serves as a diagnosis for homosexual people who feel conflicted about their sexual orientation.
DSM-III (1980)
In the third edition of the DSM, the former category “Disturbance of Sexual Orientation” is replaced by the new label “Egodystonic Homosexuality,” assigned to those whose sexual orientation caused them distress and who had a desire to change it.
DSM-III-R (1987)
During the DSM-III revision, Egodystonic Homosexuality was eliminated as a diagnosis. However, it is still possible to assign a diagnosis to people who experience persistent discomfort caused by their sexual orientation. For this purpose, this reality is included within “Sexual Disorders Not Otherwise Specified”, a broader category.
DSM-IV (1994)
As of the fourth edition of the manual, any allusion to homosexuality as a mental disorder is completely eliminated because sexual diversity is seen as part of normal human variation. Suffering related to one’s sexual condition no longer has a specific category, as it is understood that a specific label for people with non-normative sexual orientations can be stigmatizing and that a person can suffer for many different reasons, so it is not necessary to create so many subcategories.
Implications and conclussions
Although the chronology presented above summarizes the technical changes seen in the different editions of the manual published by the American Psychiatric Association, it must be said that these changes were clearly influenced by the harsh criticisms that the above-mentioned diagnoses received. The professionals who created these diagnostic categories were questioned, among other things, due to the poor scientific evidence provided by the theories on which they justified them.
I consider it is very important to recognize the work of those who, both inside and outside Psychology and Psychiatry institutions, helped facilitate these changes.
Thank you to those who maintain a critical attitude towards institutions and those who understand that science and its practical applications are influenced by the social realities of their time.
About the author
Jorge Jiménez Castillo is a psychologist at SINEWS, where he practices in English and Spanish. He works daily with local and international populations and has a long history of studying the reality of the LGTBIQ+ community in and out of the clinic. He works from a cognitive-behavioral approach with evidence-based interventions and believes that in order to provide quality psychological care one must be aware of the inequalities that intersect with users and explore how they intersect with each other.
Sinews MTI
Psychology, Psychiatry and Speech Therapy
What is Academic Support and What Does a Support Therapist Do?
The educational field today faces significant challenges. After the COVID-19 pandemic, various studies have shown negative consequences on the cognitive development and academic learning of children worldwide. This has been reflected in the complexity and diversity of learning needs, requiring new approaches for each student. In this context, the role of the educational support therapist becomes crucial to ensure proper learning development and overcome any difficulties that may arise. We generally understand their professional work, but we are often unclear about the scope of their professional competence. So, what exactly is an academic support therapist?
The Importance of the Academic Support Therapist
Academic support therapists or psychologists are professionals specialized in the educational environment of children and adolescents, focusing on analyzing special needs and learning difficulties to design strategies aimed at acquiring skills and abilities. With this objective, the academic support therapist studies the difficulties encountered, determines, and provides a series of tools, which are individually adapted to help and foster the development of their learning.
The work of the educational support therapist begins with «Understanding,» which means identifying and understanding the underlying causes of the difficulties students face. This initial understanding is fundamental, as it allows for the precise design of procedures and strategies to effectively address these difficulties. To achieve a holistic understanding of the students, brief reports and evaluations are used, providing a broader view of the student’s educational needs.
This comprehensive approach is key to their professional execution, as it allows the support therapist to develop individual interventions that address not only the surface symptoms but also the root causes. From this point, strategy planning begins, adapting to the student’s academic curriculum. These strategies are primarily implemented in learning areas that pose difficulties and where the student lacks sufficient resources for proper coping. In this regard, the support therapist provides specific tools tailored to the identified needs.

Psychopedagogical Support: Beyond Cognitive Aspects
Psychopedagogical support has its roots in cognitive psychology, initially focusing on learning difficulties, especially those related to executive function regulation. However, after the COVID-19 pandemic, support needs have been significantly exacerbated.
Functions like planning, inhibition, and working memory have suffered cognitive deterioration after the confinement period. Additionally, new adaptation difficulties to education have emerged: anxiety became a significant trigger within the adolescent and even child educational landscape. This symptomatology impacted these functions, particularly working memory, due to anxiety caused by confinement, directly affecting reading and writing performance as they are key to processing.
Therefore, we must consider that today, psychopedagogical support is not limited exclusively to cognitive functions. It is essential to understand the relationship between emotional and cognitive factors that affect a child’s development. These factors constantly interact in the execution of their skills, directly reflecting on their performance. A clear example is the common situation of facing a difficult exam and experiencing what is popularly known as a «blank mind.» These paralysis symptoms, loss of control, and insecurity are nothing more than anxiety states caused by emotional symptoms, demonstrating how emotional management can facilitate or complicate the execution of our skills and the application of our knowledge.

Current Challenges in the Educational Field
The educational context reflects what develops outside of it. After the confinement period, the COVID-19 pandemic has imposed significant challenges on the educational system:
1. Impact on the Socio-Demographic Framework:
The adaptation effort of education during the confinement period relied heavily on technological resources, which were limited for part of the school population. This lack of access has hindered the schooling period, reflecting predominantly negative effects on learning and development processes, especially in contexts with fewer economic and cultural resources. This period has further highlighted social inequity, exclusion, and educational barriers that many children and young people face, underscoring the importance of education from a more inclusive and equitable perspective.
2. Role of Teachers:
It is crucial for teachers to reflect on how they can contribute to reducing learning barriers, both cognitive and affective-motivational. The pandemic has highlighted the importance of supporting teachers and strengthening the pedagogical use of technological tools. However, there is the challenge of improving the effectiveness of training, as many teachers find it difficult to use new tools. It is necessary to promote training programs that facilitate the use of flexible strategies for a variety of students and teaching contexts. Masland’s (2021) proposal on resilient pedagogy, which meets psychological well-being needs such as autonomy, competence, and affiliation, can be an effective model to increase motivation and engagement.
3. Challenges for Parents:
Parents also face challenges, such as reviewing and modifying practices that negatively affect their children’s learning experiences. The current most prevalent issue is the excessive use of video games, cell phones, and television, which can exacerbate learning and development difficulties. Conversely, practices that promote reading, sports, and the arts should be encouraged, as they facilitate other types of learning and improve self-esteem and self-concept by developing competence strategies. Additionally, reward mechanisms are highly motivated by prizes, neglecting the practice of intrinsic motivation. The practice and discovery of this motivation foster more resilient development and improve frustration management.
4. Preparation of Educational Institutions:
Educational institutions must prepare for the return to classrooms with flexible mechanisms to design recovery and learning acceleration courses, as well as emotional support programs for students and teachers. It is essential to implement policies that allow reasonable adjustments so that students can equitably access resources and opportunities, evaluating possible losses in learning and development. These adjustments should seek to level students in cognitive, emotional, and social aspects.

Future Lines of Action for Support Therapists
Given the current challenges in the educational field, it is essential for professionals to analyze new lines of action and reflect on the measures and practices implemented. The pandemic caused a readjustment of previously established routines, incorporating new methodologies and resources. It is crucial to critically evaluate how students are adapting to these changes. Some of these lines of action include:
- Evaluating the Use of Technology: Investigating whether teachers' efforts to use and adapt to technology have facilitated effective knowledge construction processes and whether this benefits all students. It is important to adapt technology as a tool and not as the primary basis on which educational quality rests.
- Sustainability of Adapted Practices: Examining to what extent changes and adjustments in teaching practices are maintained after returning to in-person learning. Developing a routine adapted to new student needs will be crucial for development.
- Learning and Psychoeducation in the Family: Investigating the informal learning that has taken place in families during the pandemic and post-pandemic, identifying which of these are beneficial or harmful to cognitive, social, and emotional development. Professionals must guide and provide orientation in dynamics to promote improvement in different parenting styles and offer psychoeducation on new needs within the educational framework.
- Experiences and Meanings of the Pandemic: Exploring students' experiences and the meaning of the pandemic and how it has affected them within the educational system to establish new support programs that improve their impact on learning.

The pandemic has transformed the educational landscape, presenting challenges that require innovative and adaptive responses. Academic support therapists play a crucial role in this new context, helping students overcome cognitive and emotional barriers exacerbated by the health crisis. By reflecting on these new needs and adjusting our practices, we can work towards a more equitable, inclusive, and effective education for all students. The role of the therapist goes beyond cognitive reinforcement; they are the support link that will help steer in the same direction.
Written by:
Paula Taguas Labrador
Sinews MTI
Psychology, Psychiatry and Speech Therapy
Autism Spectrum Disorder and Pathological Demand Avoidance
What is “demand avoidance” and when is it pathological?
We all experience “demand avoidance” at times, i.e. we resist doing something which is either requested of us or expected of us. This article sets out to raise awareness of and explore a specific “condition” or profile which has been identified in the field of Psychology but about which there is still some controversy and lack of understanding. The focus here is on children. Recommended strategies to support PDA sufferers, both at home and in education, are also outlined.
Demand Avoidance in People with ASD
People with Autism Spectrum Disorder (ASD) sometimes avoid situations which cause them anxiety or give them sensory overload as well as activities which are not in their usual routine. They also sometimes resist transitioning from one activity to another or avoid activities which seem pointless to them. They may refuse, have an emotional crisis or try and “escape”.
How does Pathological Demand Avoidance differ from the above?
Individuals with PDA might avoid the above situations for the same reasons. However, PDA has some unique aspects:
- Many everyday demands are avoided simply because they are demands. It is the expectation (from someone else or yourself) which leads to a feeling of lack of control, and this feeling triggers anxiety increases and even panic.
- There can be an ‘irrational quality’ to the avoidance – for instance, a seemingly dramatic reaction to a tiny request, or the feeling of hunger inexplicably stopping someone from being able to eat.
- The avoidance can vary, depending on an individual’s capacity for demands at the time, their level of anxiety, their overall health/well-being or the environment (people, places and things).

What kind of everyday demands are we talking about?
- A direct demand (an instruction like “brush your teeth!” or “put your coat on!” or “do your homework!”).
- An internal demand (e.g. willing yourself to do something or bodily needs, e.g. the need to eat when you are hungry).
- An indirect or implied demand (including any expectation, for example a question that requires an answer, food that you are expected to eat, or a bill that needs to be paid.
Conversely, a demand that triggers stress or anxiety in individuals with PDA is not necessarily something unpleasant: it could be, for instance, opening your presents on your birthday.
When was the PDA profile first identified?
The term was originally coined by Elizabeth Newson in the 1980s but it took until 2003 for it to appear in formal scientific research (Newson et al., Arch Dis Child 88:595–600, 2003). Originally, PDA was a term used to describe a group of children who did not fit into the stereotypical presentation of autism recognised at that time but who shared certain characteristics with each other, the key one being a persistent and marked resistance to demands. According to Newson, autistic children display rigidity through rules, routine and predictability; in PDA their rigidity is in their need to avoid demands and control situations, which can often lead to the child appearing extremely impulsive in their emotions and behaviour, as they react to what they perceive to be demands.
Whilst autistic children often show little or no sociability, children with PDA display surface sociability. However, they often fail to recognise boundaries and struggle to understand the social norms of relationships. Children with PDA, like autistic children, often experience early language delay but often catch up later. They might have normal facial expressions and make eye contact; however their speech content can seem odd and, importantly, communication can be significantly affected by demand avoidance. The predominant characteristic of children with PDA is their continued resistance and avoidance of the ordinary demands of life. Whilst autistic children can be reluctant to comply, this is often in a non-social way; they lack the empathy to make excuses or develop strategies for avoidance. In contrast, children with PDA develop multiple strategies of avoidance, which they are able to adapt to the adult involved and can appear socially manipulative. (Newson, 2000).
Outside the UK, there is little awareness of PDA. However, in the UK, the term has been given some attention in TV and social media and this has led to an increase in pressure to consider PDA as a diagnosable disorder. Currently, while PDA is mentioned in latest edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) it is treated as a specific profile under the umbrella diagnosis of autism spectrum disorders (ASD). However, this does not mean that clinicians cannot use PDA as a descriptive diagnosis alongside a clinical diagnosis of ASD.

How common is PDA?
We don’t know. Because demand avoidance is currently understood as one characteristic in a person’s neurodevelopmental profile and is neither a diagnosable stand-alone condition nor is there a standardised assessment for the characteristic, there are no data to reliably indicate how common it may be. Research to date has been limited and often unreliable.
“Can’t” versus “won’t”: the difference between PDA and Oppositional Defiant Disorder
It is without doubt very stressful for parents to experience their child avoiding simple tasks or refusing to follow rules or basic routines. However, it is essential that we distinguish between PDA (Pathological Demand Avoidance) and ODD (Oppositional Defiant Disorder). Whereas PDA is an anxiety-driven need to be in control and avoid demands or expectations, ODD is characterised by angry and irritable mood, an argumentative and defiant attitude and vindictiveness.
Accurately identifying whether a child has PDA or ODD is key for implementing the right support strategies and can help others outside the immediate family to better understand the child’s needs. Some key characteristics of PDA which can help us with this distinction are:
- Difficulty tolerating uncertainty or unpredictability;
- Language delay and trouble with social interaction, which is common among autistic children;
- Mood swings and emotional dysregulation;
- Impulsivity and risk-taking behaviors;
- Obsessions and compulsions related to control or avoidance.
Tactics PDA children might use include distraction, making excuses, or shifting blame to avoid tasks and maintain a sense of control over their surroundings. Understanding these coping mechanisms is crucial for designing effective strategies to support them in managing their anxiety-driven behaviours.

How might a PDA child behave in a school environment?
It is possible that approaches used by teaching or special needs staff for autistic children can be ineffective for a PDA child and might even make things more difficult. In a school setting:
- They may have poor self-esteem, although this might not be obvious from their behaviour.
- Like many young people with ASD, they may behave very differently at home and school due to masking
- They may find regulating their emotions very challenging.
- A PDA learner may not seem interested in ‘doing well’ and may respond negatively to praise, for example by destroying work.
- They may say that the work is boring, or that they already know it.
- They may use charm, imaginative talk or attempt to shock to avoid demands.
- They are likely to want to build friendships with peers, but may find maintaining friendships difficult due to a need for control.
In terms of school attendance:
- They may have experienced school exclusions, even from an early age.
- A PDA child or young person may be absent from school altogether. 70% of PDA learners are either not in school or regularly struggle to attend. Many PDA children are home educated.
- Not every PDA child will have attendance difficulties – some may have slipped under the radar completely.
Support strategies for Parents at home
Unfortunately, there is limited research on support strategies. However, it is evident that people with PDA are best supported with strategies and approaches personalised to their specific strengths and needs.
The following advice is compiled from an American organisation called Trails Carolina (Trails Carolina – Leading Wilderness Therapy For Teens and Adolescents) and the Autism Society, U.K.:
- reduce and/or remove demands whenever possible;
- a collaborative approach is likely to work best, where the child is treated as an equal, rather than adults acting as an authority;
- use indirect communication styles (rather than making demands directly)
- avoid potential stressors such as eye contact, touch and confrontational postures/physical stances;
- if the child is distressed, give them space, remove spectators or move the child to a quiet space if possible;
- a coordinated approach to support is essential, involving the child, their family, school and health or social care professionals;
- In addition, it has been suggested that people with PDA may benefit from:
- identifying and understanding their demand avoidance and its triggers;
- sensory regulation and creating a sensory environment that works for them;
- therapy, counselling, mindfulness and meditation.

Support Strategies for School or Education
- Focus initially on building relationships and trust with a key adult before learning is attempted.
- Focus on the end goal rather than the means of getting there.
- Collaborate with the learner, adopting a child-centred approach focusing on their needs and strengths, and negotiating with them.
- Allow PDA learners to follow their interests and passions, and ensure learning topics are useful, meaningful and relevant to their lives.
- Provide choices and options over what work is completed, when, where, how and with whom.
- Try to recognise any signs of escalation of stress or anxiety and address them before the student reaches crisis point. Distress is usually caused by emotional, social or sensory overload; be aware of the child or young person’s potential triggers.
- Avoid direct requests; use a tone of voice and phrasing so that requests are made indirectly and allow for flexibility.
- Keep expectations to a minimum so that you can focus on the ones that are really important. This may mean having to be flexible about, for example, uniform, timetabling, homework expectations and the way results and progress are recorded.
- Provide a quiet area such as a calm corner for learners to use when they feel overwhelmed.

Some of these approaches may require significant adjustments on the part of the school, but they could be essential in ensuring that a PDA child continues to attend school.
The ongoing debate about PDA
Finally, it is necessary to highlight that, within the autism community (which includes autistic people and their families, autism researchers, health care professionals and education professionals) there is a great deal of disagreement about the validity and usefulness of the concept of PDA. However, one point on which there is broad agreement is that more and better research into Pathological Demand Avoidance is required.
Resources on PDA for Teachers and Parents
- Twinkl has partnered with the PDA Society to provide some helpful guidance documents (PDA PANDA Approach: Disguise and Manage Demands | Twinkl)
- The Autism Society (Demand avoidance (autism.org.uk). This page includes some real-life experiences in the form of quotes.
Abouth the author
Julia Jakubovics is from the UK. She has lived in Spain for over 20 years. She has a degree in Psychology and recently completed a Masters course in Interventions for Learning Difficulties in Children at ISEP (Instituto Superior de Estudios Psicológicos). She is currently working as a Shadow Teacher and Study Coach for Sinews, providing one-to-one and in-class support for children with special education needs.
Sinews MTI
Psychology, Psychiatry and Speech Therapy
What is narrative therapy and how can it help me?
Narrative therapy is a form of therapy that is based on the idea that people are the storytellers of their own lives and that by changing the way they tell their stories, they can also change the way they perceive themselves and the world around them. In this article, we will explore in depth what narrative therapy is, how it works, and how it can help us.
What is Narrative Therapy?
Narrative therapy is a form of therapy that focuses on the narration of personal stories and the exploration of how those stories affect a person’s life and experiences. It was developed by Australian therapist Michael White and New Zealand therapist David Epston in the 1980s. Narrative therapy is based on the idea that people construct their identities through the stories they tell about themselves and that these stories can be modified to promote change and personal growth.
Key Principles of Narrative Therapy
Narrative therapy is based on several key principles that guide the therapeutic process:
- Externalization of the Problem: One of the central principles of narrative therapy is externalizing the issue. This involves separating the problem from the person, allowing the person to see the problem as something external to themselves and, therefore, easier to address and change.
- Co-construction of Alternative Stories: Instead of accepting a single narrative about their lives, clients are encouraged to explore and co-create new alternative stories that may help them reinterpret their experiences in a more positive and empowering way.
- Respect for the Client's Experience: Narrative therapy believes in respecting the client's experience and the importance of allowing people to tell their own stories in their own terms. This involves active listening, validating the client's experiences, and working collaboratively with them to find solutions that are meaningful to them.

Why is Narrative Therapy Healing?
Narrative therapy is considered healing for several fundamental reasons that are rooted in its approach and therapeutic practices. Here are some key reasons why narrative therapy is perceived as a healing form of therapy:
1. Identity Reconstruction:
Narrative therapy allows people to reconstruct their identity by challenging dominant narratives that may be contributing to their emotional distress. By changing the way personal stories are told, clients can develop a more compassionate and empowering understanding of themselves, contributing to a renewed sense of self-esteem and self-acceptance.
2. Empowerment Promotion:
Narrative therapy promotes empowerment by focusing on the individual’s strengths and resources. Through the co-construction of new alternative stories, clients discover that they have the ability to influence the direction of their own lives and to face challenges with resilience and creativity.
3. Redefinition of Past Experiences:
By rewriting past stories from a more positive and empowering perspective, narrative therapy helps people find new meanings and lessons in their past experiences. This can lead to greater acceptance and inner peace regarding past events that may have previously caused distress or emotional pain.
4. Encouragement of Self-Reflection:
Narrative therapy encourages self-reflection by inviting individuals to examine their own stories and narratives in a more conscious and reflective manner. This process of self-exploration can lead to greater self-awareness and self-understanding, facilitating personal growth and positive change.
5. Building Meaningful Relationships:
The therapeutic relationship in narrative therapy is based on respect, empathy, and collaboration. This genuine connection between therapist and client provides a safe and supportive space where individuals can explore their personal stories and work together to find meaningful and lasting solutions.

Applications of Narrative Therapy
Narrative therapy has been successfully used for a wide range of issues and populations, including:
- Depression and Anxiety: Helps clients reconstruct negative narratives about themselves and find new ways to relate to their emotions.
- Trauma: Allows trauma survivors to rewrite their stories of survival and resilience.
- Family Conflicts: Facilitates communication and conflict resolution within families by helping members understand and redefine their relationships.
- Identity Issues: Helps individuals explore and assert their unique identity in the face of social and cultural pressures.
Examples of Narrative Therapy Exercises
Here are some examples of tools employed in narrative therapy:
- Self-Compassion Letters: This exercise involves the client writing a letter to themselves from a compassionate and understanding perspective. In the letter, the client can gently express their feelings, acknowledge their strengths, and remind themselves that they are worthy of love and acceptance, even in times of difficulty.
- Strengths Family Tree: The therapist guides the client in creating a family tree that represents the strengths and resources that have been passed down through generations. The client can reflect on the strengths of their ancestors and consider how these positive qualities have influenced their own lives.
- External Observer: The client takes on the role of an external and objective observer to examine their own experiences from an emotional distance. This can help the client gain a new perspective on their problems and separate their personal identity from the events and circumstances that have occurred in their lives.
- Life Book Creation: The client creates a life book that includes significant moments, achievements, and experiences that have shaped their identity. By reflecting on these events and narratives, the client can identify common patterns and discover new ways to interpret their personal story.
- Gratitude Journaling: The client keeps a gratitude journal where they record things they are grateful for each day. This exercise fosters a more positive and appreciative approach to life and helps the client recognize the good things that exist amidst challenges and difficulties.

In conclusion, narrative therapy is a powerful tool that can help people reconstruct their life stories and find new ways to relate to their experiences. By changing the way they tell their stories, people can change the way they perceive themselves and the world around them. Whether facing depression, overcoming trauma, or navigating family conflicts, narrative therapy offers a client-centered approach that promotes meaningful and lasting personal change and growth,
Abouth the author
Verónica Sarria is a health psychologist at Sinews. She is specialized in eating disorders and obesity, working with adolescents and adults. She also treats other problems such as anxiety, depression, grief, self-esteem and interpersonal relationship problems, among others. Her orientation is cognitive behavioral but she integrates tools and techniques from other currents according to the needs of each patient, thanks to her training in mindfulness, mindful eating, attachment theory and systemic (family) therapy.
Sinews MTI
Psychology, Psychiatry and Speech Therapy











